Questions for your Breast Surgeon and Plastic Surgeon:
- Am I a good candidate for breast reconstruction?
- What type of reconstruction do you recommend?
- Am I a candidate for a nipple-sparing or skin-sparing mastectomy?
- What are the complications and disadvantages of reconstruction?
- What are the advantages and disadvantages of a bilateral mastectomy?
What is Breast Reconstruction?
Breast reconstruction is commonly performed after a mastectomy. The goal is to re-create the shape of the breast with one or multiple surgeries by a plastic-reconstructive surgeon. Today, the cosmetic results are leaps and bounds beyond where they were just a decade ago. With that said, breast reconstruction is far more complex and carries much higher complication risks than an elective breast augmentation. About half of women who have a mastectomy in the United States will undergo breast reconstruction.
A mastectomy without reconstruction is also a surgical choice. One can wear a breast prosthesis and avoid the more extensive surgeries and risks of complications with a reconstruction. The decision to have breast reconstruction is complicated and personal. It is important to realize that everyone has different goals, different personal situations, and their own reasons as to how they manage their unique breast cancer situation.
Treating your breast cancer comes first.
There are many complex factors your breast cancer surgeon must consider about your reconstruction options. Most of the time your reconstructive options are not affected by your cancer treatment. But if you do have a complex breast cancer situation, ask your surgeon to present your dilemma to a multidisciplinary conference for further input from other surgeons, medical oncologists, and radiation oncologists. Balancing a great cancer outcome with a good cosmetic outcome sometimes requires intensive discussions amongst your breast surgeon’s team of breast cancer specialists.
Cancer treatments that affect your reconstruction:
- Chemotherapy can change the timing of surgery and reconstruction
- “Post Mastectomy Radiation Therapy” can alter options
- Radiation of a reconstruction can change cosmetic outcomes
- Genetic testing before surgery can help decision-making
- Better cosmetic outcomes with when a mastectomy and reconstruction begin together
A surgical “Team Approach” is best.
Your breast surgeon will likely guide you to a plastic-reconstructive surgeon he or she works with regularly. They will work as a “team” to plan the best surgical approach to your cancer and likely work together the day of your mastectomy to begin your reconstruction. Subsequently, the plastic surgeon works with you in planning further staged reconstruction and revision surgeries. This partnership is important to ensure you get the best cancer and cosmetic outcome possible.
What are your Breast Surgeon’s “Mastectomy Options”?
A skin-sparing mastectomy preserves the skin of the breast but not the nipple or areola. Preserving the normal “skin envelope” in the shape of your breast leads to better cosmetic results.
A nipple-sparing mastectomy preserves all the skin of the breast including the nipple and areola. If you have an early stage breast cancer located away from the nipple you may be a candidate for this approach. Nipple-sparing mastectomies generally lead to the best cosmetic results. Women with very large breasts may not be appropriate for a nipple-sparing technique.
A traditional mastectomy saves only enough skin to cover the chest wall. Sometimes this is required to effectively treat the cancer. Reconstruction can still be performed in this setting, but the cosmetic results may not be as successful as nipple-sparing or skin-sparing approaches.
What are your Plastic Surgeon’s “Breast Reconstruction Options”?
Two-stage implant reconstruction involves implantation of a “tissue expander” implant at the time of your mastectomy to help mold and stretch the skin to the desired size and shape. This implant will be expanded one “fill” at a time at office visits until the desired result is achieved. At a second operation, the plastic surgeon will remove the expander and place a permanent implant filled with “saline” or “silicone.” This the most common approach to breast reconstruction today.
One-stage implant reconstruction occurs with well-selected patients that can undergo placement of the “final implant” during the mastectomy surgery. This approach is not nearly as common as the two-stage approach outlined above.
Tissue flap reconstruction is used in about 10% of all breast reconstructions in the United States. The benefit is that it uses a segment of your own tissue from your abdominal area or your back to fill the space needed to reconstruct the breast. It is a much more complicated and involved surgery but the results seldom require surgical revisions in the future. Types of tissue flaps include DIEP flaps, TRAM flaps, and latissimus flaps.
Does reconstruction hide cancer recurrence?
Research has not shown that a reconstruction will hide a breast cancer recurrence. The overall chance of cancer recurring in the site of the mastectomy (local recurrence) in early stage breast cancer is about 3% over five to ten years. If cancer does recur, it generally is detected near the breast incision as a small lump. Annual mammograms are not needed after a mastectomy and reconstruction. Reconstruction does not hide cancer recurrence from view any more than a mastectomy without reconstruction.
What are “disadvantages” of a bilateral mastectomy and reconstruction?
- Surgical complication risks are slightly increased
- Loss of sensation in the skin of both breasts
- Increased need for revision surgeries in the future
- Does not improve your “overall survival” from breast cancer
- Does not lessen the chance you will need chemotherapy
- A chance you might regret the decision in the future
What are “advantages” of a bilateral mastectomy and reconstruction?
- Lessens the chance of developing a new cancer in either breast
- Screening mammograms are no longer needed
- Cosmetic outcomes are much improved over the last decade
- Reconstructing both sides may result in matching breast appearance
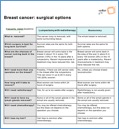
This “Option Grid” (here) is an excellent resource that outlines your Breast Reconstruction Surgery Options:
Patient-Friendly References:
This website covers multiple topics about breast reconstruction (here). Toggle through their Table of Contents on this page for specific information. The American Society of Plastic Surgeons is the largest plastic surgery specialty organization.
There is excellent information about “Breast Reconstruction after Mastectomy” (here). The National Cancer Institute is a government agency dedicated to distributing information to the public about cancer and cancer research trials.
Review their page on “Breast Reconstruction” (here). There is excellent detail about all of your surgical options on this website. This site is created for patients by the American Society of Breast Surgeons.
This outline on “Breast Cancer: Surgical Options” (here) is a cutting-edge presentation of the differences between a lumpectomy and a mastectomy. The Option Grid Collaborative is one of the largest developers of clinical decision aids, based at the Dartmouth Institute for Health Policy and Clinical Practice.
This excellent outline mentioned above and (here), “Breast Reconstruction after Mastectomy” is a presentation of the differences between a lumpectomy and a mastectomy. The Option Grid Collaborative is one of the largest developers of clinical decision aids, based at the Dartmouth Institute for Health Policy and Clinical Practice.
This is a detailed outline (here) of treatment options for women with breast cancer, written specifically for patients. Choose the brochure that best reflects your own unique situation. The NCCN is a consortium of organizations and governmental agencies to promote quality breast cancer care.
More Detailed References:
If you want to get deep into the details, this free 200-page pdf document (here) has guidelines to help clinicians to make treatment recommendations about nearly all aspects of breast cancer. You can easily register (here) as a non-professional to get access and more information about breast cancer. The National Comprehensive Cancer Network is the leading organization in developing clinical guidelines.